Cancer To-Do List
tests
answers through tests
You have probably already experienced a variety of testing — initial tests, scans, bloodwork, imaging, follow-up tests, and the list goes on. Once you get through the initial tests and have an accurate assessment of your diagnosis, then it’s time to get to the possible root causes.
Work with your medical team to assess your health status through testing. Testing may identify underlying issues such as: digestion difficulty, cardiovascular issues, endocrine and exocrine imbalance, musculoskeletal issues, immune imbalance, inflammation, and poor detoxification. These issues may be keeping your body’s systems from performing optimally.
Once you have the big picture of your situation, including diagnosis and treatment plan, it’s time to move forward with the plan of action. Do this with confidence, and don’t let the numerous tests you will undergo take you on a roller coaster. Instead of being controlled by the emotions that come with the results of a single test, step back and look at the bigger picture of the combined test results and the trends they are showing you. Regardless of test results, stay committed to a healthy lifestyle. Underlying issues are best addressed not with more testing, but with prevention.
Before you review this page, I want to remind you that blood work or diagnostic tests, like scans, often make you feel out of control, and invite you to worry. Try to remember that tests are not always a true reflection of what is going on in the body. Pray and focus on forming a strong daily routine of basic health habits. That is something you can control!
-
Learn about the most commonly used medical tests and procedures, along with the anxiety that may accompany those tests.
-
Use testing to determine the health and function of basic biomarkers of the body in an effort to reveal root causes.
-
Learn about blood tests, how they can help to identify underlying issues, and help to monitor your progress moving forward. Gain an understanding of three basic blood tests routinely run by oncologists: CBC, CMP, and tumor markers.
-
-
Learn about a blood test that identifies a specific inherited cancer-causing gene; along with the science of epigenetics, a science that offers good news about gene expression.
-
My journey with hormones and what I learned including testing hormones, hormonal imbalance, and balancing hormones for better health.
Every three months for the first five years, Joel picked up his chocolate drink to prep for a CT scan as part of his surveillance. Unfortunately, in the months and weeks leading up to the test, there was “scanxiety.” We thought we made up that word, but apparently it is quite popular, and we understand why. Learning you have cancer comes as such a shock, and you may feel on edge for quite some time. As follow-up tests roll around every few months, the scanxiety may set in. Eventually, you become a little desensitized to it . . . well, kind of. :)
Over the course of my journey, my oncologist ordered a few ultrasounds for lumps she had found under my arms. The first one was a little disconcerting, but I was less anxious on each subsequent test. Another oncologist recommended that I have a PET scan once a year as part of my follow-up, but I decided against it. The reason is that even if the scan showed something, I would do the same thing I’m doing now. I’m already implementing all the lifestyle habits I can to achieve optimal health. I’m not recommending this as a course of action for everyone, but based on my personality, this is what suits me best.
Joel and I met a dear friend on our journey who has stage 4 head and neck cancer. He suffered from extreme scanxiety, so finally he discontinued the scans. He felt the pre-scan anxiety was probably weakening his immune system, so he just hit a stopping point.
Everyone is going to respond differently to follow-up tests depending on personality, life responsibilities, and faith. For me, two things have helped me feel better about saying no to some of the scans and tests listed below: 1) my commitment to a daily routine of basic health habits, and 2) leaning on the Lord Jesus Christ, that helps me put all anxiety behind me.
Below are some of the most commonly used medical tests and procedures.
Scanxiety
X-RAys
X-ray was the very first diagnostic imaging tool and is the most common diagnostic imaging exam performed. It is usually the first test to be requested by doctors. X-rays involve targeting radiation to a certain area of the body where images are needed. These images show structures inside your body like bones, chest obstructions, etc.
Ct scan
A CT (computed or computerized tomography) scan combines a series of X-ray images taken from different angles around the body, and uses computer processing to create cross-sectional images (slices) of the bones, blood vessels, and soft tissues inside the body. This kind of motion picture X-ray exposes you to considerable ionizing radiation. Even though there are risks of radiation, the CT scan is quite common and was the best option for Joel's follow-up, because CT scans see specifics in the body more accurately than an MRI or other tests. https://www.consumerreports.org/cro/magazine/2015/01/the-surprising-dangers-of-ct-sans-and-x-rays/index.htm
Mri
MRI (magnetic resonance imaging) is a medical imaging technique that uses a magnetic field and computer-generated radio waves to create detailed images of the organs and tissues in your body. If your doctor offers an MRI instead of CT scan, take it! There is a big difference between the two in terms of radiation exposure. An MRI does not involve any ionizing radiation, but instead relies on giant magnets to get a good look at an area of the body. I have had breast and brain MRIs.
Pet scan
A PET (positron emission tomography) scan is an imaging test that can help reveal the metabolic or biochemical function of your tissues and organs. The PET scan uses a radioactive drug (tracer) to show both normal and abnormal metabolic activity. According to the Mayo Clinic, “Cancer cells show up as bright spots on PET scans because they have a higher metabolic rate than do normal cells . . . PET scans must be interpreted carefully because noncancerous conditions can look like cancer, and some cancers do not appear on PET scans.” Even though a PET scan is not exact, it can often detect cancer before the disease shows up on other imaging tests, such as CT (computerized tomography) and MRI (magnetic resonance imaging). My oncologist calls the PET scan a "truckload of radiation" and she seldomly uses this test due to the harmful effect to the body.
Ultrasound
A diagnostic ultrasound, also called sonography or diagnostic medical sonography, is an imaging method that uses high-frequency sound waves to produce images of structures within your body. The images can provide valuable information for diagnosing and treating a variety of diseases and conditions. Ultrasounds are generally considered very safe, non-invasive, diagnostic procedures. It is a form of electromagnetism.
COLONOSCOPY
A colonoscopy is an internal exam to detect changes or abnormalities inside the large intestine (colon) and rectum. In one study, complete colonoscopy was strongly associated with fewer deaths from left-sided colon cancer, but not from right-sided. https://pubmed.ncbi.nlm.nih.gov/19075198/ https://pubmed.ncbi.nlm.nih.gov/36214590/
Joel had not had a colonoscopy since he had just turned 50, and he did have left-sided colon cancer. Joel did a fecal smear (a laboratory test of a stool sample) the year before he was diagnosed. The test came back normal, with no indication that he had colon cancer. Joel is encouraged to have one colonoscopy each year.
Here is some information regarding screening data on colonoscopies: https://pubmed.ncbi.nlm.nih.gov/11678550/
Pap Smear
A Pap (Papanicolaou) smear, also called a Pap test, is a procedure to test for cervical cancer in women. A Pap smear involves collecting cells from your cervix — the lower, narrow end of your uterus that sits at the top of your vagina. A Cornell cytologist, named George Papanicolaou, discovered this test to find precursor cells in asymptomatic women so they could receive treatment for pre-cervical cancer. However, Gilbert Welch, M.D., in his book Should I Be Tested for Cancer, explains that "atypical squamous cells of unknown significance (ASCUS) and squamous intraepithelial lesion (SIL) almost never become cervical cancer and a positive result is more likely to be a false positive than to be cancer." A study in Sweden showed that women whose cervical cancers were found by a Pap smear had a 92% cure rate. https://pubmed.ncbi.nlm.nih.gov/18445828/
Mammogram
A mammogram is an X-ray image of the breast. This procedure exposes the breasts to radiation. Doctors use mammograms to look for early signs of breast cancer. However, mammograms miss about 1 in 8 breast cancers and have limitations. https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/mammograms/limitations-of-mammograms.html
3D mammography (also called called breast tomosynthesis) is an FDA-approved, advanced technology that takes multiple X-rays of breast tissue to recreate a 3-dimensional picture of the breast. Traditional mammography obtains just a single image.
My cancer center, Christine E. Lynn Women’s Health & Wellness Institute, says “There’s no wonder in our BRA (Breast Risk Assessment).” They encourage women to ask themselves these questions to assess risk of breast cancer:
Have you ever been told you have high breast density?
Do you have breast implants?
Have you had a benign breast biopsy?
Have you had prior radiation to the chest area?
Do you have a personal or family history of ovarian, colon, or breast cancer?
Is there a history of breast cancer among your mother, father, brother, or sister, or at least two other close relatives?
Have you ever taken oral contraceptives, or hormone therapy after menopause?
Did you get your first menstrual period before 12 years of age?
Did you have your first child after age 30, or have you never been pregnant?
Here is some information regarding screening data on breast cancer:
https://pubmed.ncbi.nlm.nih.gov/11684218/ https://pubmed.ncbi.nlm.nih.gov/24380095/ https://pubmed.ncbi.nlm.nih.gov/24519768/
THERMOGRAPHY
Thermography is a test that uses an infrared camera to detect heat patterns and blood flow in the body. The test can be done on the entire body or just part of the body. This procedure is not invasive and does not use radiation.
Surprisingly, when I asked my CAM doctors about the validity of this test as a cancer detection tool, the response was the same with all of them, and not inspiring. I was told there is a high false-positive rate, which means results may be indicative of disease that isn't actually present. Thermography screens for cancer by detecting temperature differences in the breast. Cancer cells and tumors are warmer, but cancer is not the only reason for heat differences that are detected. Exercise, inflammation, large breasts, obesity, hormonal changes due to menstrual cycles, etc. can contribute to inaccurate readings.
These same doctors were also not fans of mammograms due to radiation. Here is Dr. Pam Popper’s opinion on both mammography and thermography, as well as her answer to reduce your risk of cancer with diet and lifestyle changes. https://www.youtube.com/watch?v=axxc6bVb33s
https://rumble.com/v2tpwz0-updated-guidelines-regarding-mammograms.html
https://rumble.com/v2v6kyu-more-about-mammograms.html
I had thermography done several times leading up to my diagnosis because I had high breast density so I did thermography alongside mammograms. Each time, my results were normal. I have done thermography three times since my diagnosis and I had normal results each time.
Above are images from one of my thermography tests. My results were normal. I was told that the red areas may indicate inflammation but not necessarily.
Breast Self Exams
It is wise to do regular breast self exams and teach your daughters to do them as well.
Unfortunately, a mammogram was not how I learned I had cancer. I had a routine mammogram each year. I was told every year that I had fibrocystic breasts and that I was at higher risk of developing breast cancer. As a result, they recommended a yearly diagnostic mammogram, which is a mammogram followed by an ultrasound. My mammogram, just ten months prior to my diagnosis, was “normal.” I found the lump in my breast between my yearly mammograms (which is usually how women find their breast cancer.) The lump felt like a frozen pea, which I quickly learned was more concerning than a soft, movable lump. A hard lump is more indicative of cancer.
I was shocked to learn that these fast-growing tumors are often the most aggressive. “Breast cancers that are first detectable in the interval between screening mammograms are more likely to be aggressive, fast-growing tumors,” according to a study published in the Journal of the National Cancer Institute. https://www.sciencedaily.com/releases/2011/05/110503161405.htm
Either they missed the tumor on my last mammogram, or the tumor may have grown within the ten-month period. One of my doctors called it an "angry tumor."
Below is an excerpt from my mammogram results showing I had "Category 5" findings, which means there is a 97% chance of malignancy.
-

December 2018
Shortly after Joel finished treatment, I had my annual mammogram. I felt higher anxiety than normal because of Joel’s diagnosis. My sister sent me this text: “It’s so difficult to learn, but it really is about relinquishing control. There are truly some things in this life that are out of our hands. Those are the times when we have to picture ourselves lying face down, prostrate before the Lord in complete surrender. When things are out of our hands, guess what? They are in HIS!”
-
Congratulations!
I had a routine mammogram, just ten months prior to my diagnosis, that was “normal.” The women’s center mailed me a letter congratulating me on my good results. I almost felt weak with relief. Joel had just finished chemo. All I wanted to do was to stay strong and healthy so that I could take care of my family and move past cancer, but little did I realize what the next year would hold.
-

October 2019
I felt a lump in my left breast. Two days later I had a diagnostic mammogram. The radiologist told me I had a "Category 5" tumor. Really? Category 5? I live in Florida where we have categories of hurricanes, and a Cat 5 storm is devastating. I need to advocate to change that name! LOL :)
Root Causes
putTING your health to the test
Assess your health in the areas below and monitor your progress over time. As you form a strong daily routine of basic health habits, you will most likely notice an improvement in underlying root causes.
ALLERGIES
According to the Mayo Clinic, “Allergies occur when your immune system reacts to a foreign substance — such as pollen, bee venom or pet dander — or a food that doesn't cause a reaction in most people. When you have allergies, your immune system produces substances known as antibodies that identify a particular allergen as harmful, even though it isn't. When you come into contact with the allergen, your immune system's reaction can inflame your skin, sinuses, airways or digestive system. The severity of allergies varies from person to person and can range from minor irritation to anaphylaxis — a potentially life-threatening emergency. While most allergies can't be cured, treatments can help relieve your allergy symptoms.”
AUTOIMMUNE
When the immune system is unable to differentiate between your own cells and foreign cells, the body mistakenly attacks normal cells. Autoimmune diseases can affect almost any part of the body, including the brain, heart, lungs, glands, digestive system, eyes, muscles, skin, joints, etc.
BLOOD PRESSURE
The pressure exerted by the blood against the walls of the arteries and veins; measurement is expressed as systolic and diastolic blood pressure readings. According to the Mayo Clinic, blood pressure readings of <120/80 mm Hg are considered in the normal range.
BLOOD CHOLESTEROL
Fat-like substance that your body needs for good health. Cholesterol comes from the foods you eat; your liver also makes cholesterol. The role of cholesterol metabolism is important for cancer patients. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6405981/
BLOOD SUGAR
Sugar in the form of glucose in the blood. The body gets glucose from the food we eat. Then the glucose enters the bloodstream and is taken up by the body’s cells with the help of a hormone called insulin. If the body doesn’t make enough insulin, or if insulin is not taken up by the cells, the blood glucose can rise, leading to diabetes. Here are the tests dealing with blood sugar:
CMP (comprehensive metabolic panel)
CMP is a chemistry panel that measures overall health of the body by assessing cardiovascular risk, metabolic function, electrolyte status, minerals important for bone health, liver and kidney function, etc. Often this test is run by doctors at random times of the day, without fasting. I explain the various parts of this test below.
Fasting glucose
Fasting glucose measures how much glucose is in the blood after at least eight hours of fasting.
Fasting insulin
Fasting insulin measures the insulin levels in the blood after at least eight hours of fasting. Insulin is a hormone that regulates the amount of glucose in the blood.
Glucose tolerance
A glucose tolerance test detects diabetes; measures how well your body metabolizes glucose by measuring how much glucose is in the blood after at least eight hours of fasting and after drinking a sugary drink. Blood is drawn over the course of several hours.
HbA1c (hemoglobin A1C)
HbA1c estimates how much glucose has been in your bloodstream over the last three months.
BODY COMPOSITION
The measurement of fat mass to lean mass. Women should strive to reduce their body fat to 18-22% of total weight, and men to 14-17% of total weight.
BODY WEIGHT
The amount of heaviness or mass.
INFECTIONS
The invasion of bodily tissue by pathogenic microorganisms (viruses, bacteria, and other germs) that can cause injury and progress to disease, even cancer.
The week before I learned I had cancer. I looked healthy, but I had root causes that needed to be uncovered.
I heard a doctor describe our approach to health like a tree. She said that we tend to treat the leaves instead of the roots. We paint the brown leaves green (with medications, etc.) instead of getting to the root of the problem (with lifestyle changes). We need to fix our root system!
ABNORMAL RESULTS
If we experience an abnormal test result, our doctors will often re-run the test either right away, six weeks later, or a few months later. Usually, the test comes back closer to normal or within the normal range; but when an issue doesn’t resolve, it is important to explore the possible reasons. When Joel was going through treatment, he had many abnormal results that we eventually concluded were due to medications he was taking. Whenever I have had a negative result, I would view it as a challenge to get that part of my health under control before the next six-week retest.
DAILY FLUCTUATIONS
I have also come to learn, from doing my own research, that if you take labs from a person at various times throughout the day, their levels can fluctuate significantly. If your doctor did not re-run the test, request that the doctor do so. A singular abnormal lab result may be very concerning to you; however, it may not elicit a response from your physician. Most doctors are interested in trends, as opposed to a single abnormal result.
Reference Ranges
Reference ranges are determined by the individual laboratory analyzing your specimen, and they vary from one lab to another. A result considered “abnormal” by one lab may be considered “normal” by another.
Blood Test Basics
THINGS TO KNOW
RESULTS over time
My oncologist and primary doctor both use Quest Diagnostics for labs, so I receive my results on that website. I can choose to see my “current” result, the “reference range,” and then my results “over time.” One of the most valuable features is when I click on the “over time” button, because I can see a graph showing my progress. That feature provided so much encouragement because it allowed me to monitor my improvement.
Tumor Markers
Tumor markers measure substances that cancer releases into the body. It is important to understand that they are not absolutely conclusive. If tumor markers are elevated, it is not always indicative of cancer; and if a tumor marker is normal, it doesn't necessarily mean that you are free of cancer. Tumor markers have not been shown to improve survival rates. Nevertheless, blood tumor marker tests are generally used by oncologists to monitor whether or not a treatment is working or has worked. Additionally, most oncologists run tumor markers at routine follow-up appointments.
Ask for baseline tumor markers if they suspect you have cancer. It’s ideal to have your tumor markers run before you have had any surgery or treatment. This way you have a baseline to compare to future test results. We wish we had known Joel’s baseline tumor marker prior to the cancer being removed. We didn't know to ask for this. The colon cancer tumor marker is called CEA. The first time Joel’s CEA was checked was after his surgery. The first time we understood the meaning of a tumor marker was during Joel’s chemotherapy. After one of his treatments, the oncologist called us that night and said that Joel's CEA tumor marker had jumped up significantly, so he ordered a PET scan for the next day. The PET scan results showed an area of concern at the base of Joel's brain, so a brain scan was ordered. Fortunately, the brain scan came back clear and Joel's chemo resumed. Since that day, Joel's CEA marker has never been in the normal range. It is a constant source of stress because he has no baseline to measure it against. We have both learned not to let tumor markers be a source of frustration, but rather a source of motivation to stay committed to self-care.
Blood tests: where to begin
-
Female Panel Blood Test
Here is basic bloodwork, plus other important lab tests for women.
-
Male Panel Blood Test
Here is basic bloodwork, plus other important lab tests for men.
Basic BLOOD TESTS
Below are the three basic blood tests routinely run by our oncologists: CBC, CMP, and tumor markers. These basic tests may be run every 3-6 months or once a year. You and your physician(s) may add other tests to this routine list, based on your individual health. For example, they may add a lipid panel if you need to monitor your cholesterol levels.
CBC (Complete Blood Count)
CBC is a general indicator of overall health. The test measures the amount and type of blood cells (red blood cells, white blood cells, and platelets). This test provides information regarding the immune system, the possibility of infection, blood disorders, the body's ability to clot, nutritional deficiencies, and more.
White blood cells (lymphocytes, monocytes, neutrophils, eosinophils, and basophils)
CMP (Comprehensive Metabolic Panel)
CMP is a chemistry panel that measures overall health of the body by assessing cardiovascular risk, metabolic function, electrolyte status, minerals important for bone health, liver and kidney function, etc.
ALP, ALT, and AST are liver enzymes:
Glucose / blood sugar - also ask for your HbA1c (hemoglobin A1C) to be tested; it measures blood glucose averages over time.
Tumor Markers
AFP (alpha-fetoprotein) - tumor marker that may be elevated in liver, ovarian, or testicular cancer; as well as liver diseases, such as cirrhosis and hepatitis.
B-cell - tumor marker for B-cell lymphoma.
BCR-ABL - tumor marker for some leukemias.
B2M (Beta-2 microglobulin) - tumor marker for multiple myeloma, some leukemias, and lymphomas.
*CA-125 (cancer antigen 125) - tumor marker for cancers of the ovary and uterus. May also signal breast cancer recurrence.
*CA 15-3 (cancer antigen 15-3) - tumor marker for breast and ovarian cancers.
*CA 19-9 (cancer antigen 19-9) - tumor marker for gastrointestinal tract cancers, such as colon, pancreas, stomach, and liver.
*CA 27.29 (cancer antigen 27.29) - tumor marker for breast cancer.
Calcitonin - tumor marker for thyroid carcinoma and C-cell hyperplasia.
**CEA (carcinoembryonic antigen) - tumor marker for cancers of the colon, lung, liver, breast, and pancreas.
CgA (Chromogranin A) - tumor marker for neuroendocrine, carcinoid, and neuroblastoma tumors.
CYFRA 21-1 (Cytokeratin 19 Fragment) - tumor marker for lung cancer and metastatic breast cancer.
DCP (des-gamma-carboxy prothrombin) - tumor marker for HCC (hepatocellular carcinoma).
Gastrin - tumor marker for G-cell hyperplasia, gastrin-producing tumor (gastrinoma).
GGT (gamma-glutamyl transferase) - tumor marker for carcinoma of the pancreas.
LD or LDH (lactate dehydrogenase) - tumor marker for testicular and other germ cell tumors.
MIg (Monoclonal immunoglobulins) - tumor marker for multiple myeloma and Waldenstrom’s macroglobulinemia.
PSA (prostate-specific antigen) - tumor marker for prostate cancer.
SMRP (soluble mesothelin-related peptides) - tumor marker for mesothelioma, a rare cancer associated with asbestos exposure.
TCR (T-cell receptor) - tumor marker for T-cell lymphoma.
*Julie’s tumor markers
**Julie and Joel’s tumor markers
Circulating Tumor Cells
Be sure to visit the Conventional Treatment page to understand circulating stem and tumor cells known as CSCs and CTCs. In summary, CTCs (circulating tumor cells) are cancer cells that are shed by a primary tumor and travel through the bloodstream of cancer patients.
CTCs have been proposed as a blood marker for cancer and an independent prognostic factor for PFS (progression-free survival). CTCs are measured through blood testing, called liquid biopsies. For now, this blood test is not part of mainstream oncology.
We had our CTCs measured several times with CAM doctors through a variety of companies.
In 2022, Joel’s oncologist enrolled him in a trial with Guardant Health, measuring CTCs for advanced cancer patients. Joel’s CTCs were measured a couple of times during this trial, and we were thrilled that his results came back with undetectable CTCs.
If you have your CTCs tested, most likely it will be with a CAM doctor.
CTC Test
Joel and I both had detectable CTCs in our blood after each of our diagnoses. We have had a few more tests, and this was my best one. I prefer to keep my mind focused on this CTC test. I love looking at “CTCs: NOT DETECTED”
Genetic Test
INHERITED CANCER GENES / FAMILY HISTORY
After our surgeries, we were both given the option to have a genetic blood test to see if we had a family history of our specific types of cancer. For Joel, this was particularly important because certain ethnic groups have a greater likelihood of carrying a cancer-causing gene. For instance, 1 in 40 Jewish people have Ashkenazi Jewish heritage, so they are more likely to have an inherited risk of colon cancer. This is called Lynch syndrome. Since Joel is Jewish, it made sense to have him tested. Fortunately, he did not have Lynch syndrome.
I decided to do the testing - simply because we went through this with Joel, and I knew the genetic doctor. I was sure it would come back negative, but surprisingly it did not. “Cancer Gene Shocker”
In the 19th century, doctors discovered that some cancers run in families; but oncologists did not embrace this idea until the 1970s. According to the National Cancer Institute, “this kind of genetic testing looks for specific inherited changes (variants) in a person's genes. Genetic testing is done on a sample of a person’s blood, saliva, or other tissue to see if there is an abnormal change (also called a mutation) in a gene that is linked to a higher risk of cancer. Genetic variants can have harmful, beneficial, neutral (no effect), unknown, or uncertain effects on the risk of developing diseases. Harmful variants in some genes are known to be associated with an increased risk of developing cancer. These inherited variants are thought to contribute to about 5 to 10% of all cancers."
Eventually, research showed that cancer genes are in all of us, but there is an on/off switch. Genes turn on in people who get cancer, and remain off in people who don’t. The science of epigenetics shows that our DNA is not our destiny, and that diet and lifestyle can change the expression of genes - even poor genes. I have heard it said another way, "Genes may load the gun, but it's diet and lifestyle that pull the trigger."
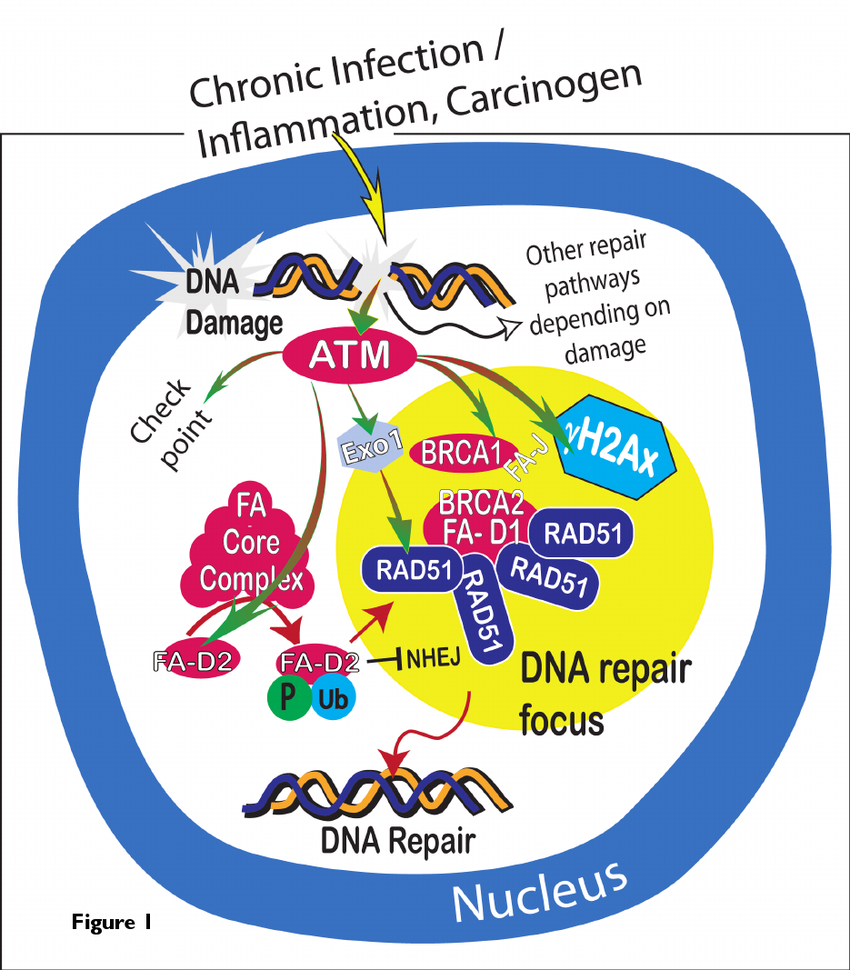
With all of the research on genetics and cancer, two significant discoveries have been made. First, it was discovered that hormone replacement therapy increases the risk of developing breast and ovarian cancers. Next, in the mid-1990s, scientists discovered two genes (BRCA1 and BRCA2 - BR=breast; CA=cancer). BRCA genes don't cause cancer directly. They increase the likelihood of mutations that can lead to breast and/or ovarian cancer.
A positive genetic test does not indicate the presence of cancer; or that a person who carries one of these genes will definitely get cancer. There is still a lot to learn about genes and the behavior of cancer. This is an area of scientific research that is getting a lot of attention.
Right after my surgery, the cancer center did a family genetics blood test. It took over a month to get the results. I had an appointment with an oncologist who handles genetics. It was a shocking moment!
RAD51D mutations are associated with an increased risk of multiple cancers. The image above is from researchgate.net.
HEALTHY HormoneS
Dear hormones, please leave when you’re done!
“ I’m not waiting for the stars to align, just my hormones.”
MY MENSTRUAL CYCLE AND PMS
The average age of menarche in rural China is 17, while the average age in the U.S. is 11. Intake of animal food, particularly dairy, increases estrogen levels, which then lowers the age of menarche. These higher hormone levels increase the rates of breast cancer. The incidence of breast cancer is five times higher in the U.S. than China. https://pubmed.ncbi.nlm.nih.gov/10981459/ https://pubmed.ncbi.nlm.nih.gov/20042466/ https://pubmed.ncbi.nlm.nih.gov/21347271/
Menstrual cycles should begin in young girls around ages 15-17. I was almost 17 when I started my menstrual cycle. I was so late that my friends in high school had the boys at school congratulate me. At the time, I was told they didn't know why they were congratulating me, but I doubt that now. :)
My periods were accompanied by terrible symptoms of PMS, irregular blood flow, and pain. Then during the time I played college sports, I didn’t have a period for almost two years. Young women participating in sports are susceptible to the female athlete triad, which is an interrelationship of menstrual dysfunction, low energy availability, and decreased bone mineral density.
Fast forward to the age of 33 when I made huge dietary changes. As a result, my painful periods and PMS went away. My menstrual cycles became normal for the first time in my life.
MY YEARLY MAMMOGRAMS
I began having regular mammograms in my late 40s. Each time, I was told that I had fibrocystic breasts, which meant an increased risk of breast cancer. Because of this, I always had a routine diagnostic mammogram, which is a mammogram followed by an ultrasound of each breast. I had a routine mammogram in December of 2018, just ten months prior to my diagnosis. I remember being overjoyed when I received my letter of congratulations, informing me that I was free of breast cancer.
MY DIAGNOSIS OF HORMONE-POSITIVE CANCER
In the year leading up to my diagnosis, my periods became irregular and I had mild spotting in between periods. I was 52, so I thought this was a perimenopausal symptom. Perhaps it was, but I shouldn’t have assumed. Perimenopause is the natural transition to menopause. The average age of perimenopause for women is 52, but it can occur any time after age 40. Keep track of your menstrual cycle so you are paying close attention to your body. Never assume it is normal to have irregular cycles.
I was 53 when I was diagnosed with 90% ER+ (positive) and 90% PR+ (positive) breast cancer. I considered myself extremely healthy — I wasn't overweight, I ate a low-fat, high-fiber, plant-based diet, and I exercised several times per week.
However, I have a gene that causes breast cancer, and my stress level was off the charts! Stress can wreak havoc on your overall health, so that is probably what happened to me.
what i’ve learned about HORMONES, hormonal IMBALANCE, AND BALANCE
“Estrogen is an essential hormone produced by women throughout their menstruating years as part of fertility. Estogen has 260 different functions in the human body, including antioxidant, maintenance of bone structure, and protection against cardiovascular diseases. Estrogen is a growth hormone and can accelerate the growth of anything, including hormone-dependent cancers. ”
Hormones serve to manage and maintain many functions of the body. There are many different hormones that control all kinds of processes including blood pressure, blood sugar, body temperature, electrolyte balance, development and growth, digestion, metabolism, mood, reproduction, sexual function, sleep, and stress. A variety of glands in our body release hormones that trigger other bodily functions. For example, the adrenal gland releases cortisol and other stress hormones; the pineal gland releases melatonin, which helps to control the sleep-wake cycle, and the ovaries release estrogen which is crucial for the development of breasts, bone formation, the widening of hips to prepare for pregnancy, and so much more. When the body is functioning optimally, hormones are in balance. Yet there are predictable and naturally-occurring points in our lives when hormones are out of balance (puberty, menstruation, pregnancy, and menopause). Healthy lifestyle habits will keep those periods of hormonal imbalance in check, whereas poor lifestyle habits will further exacerbate hormonal imbalances. As hormone levels remain too high or too low, bodily functions are impacted and side effects occur.
Hormones - Estrogen, Progesterone, and Testosterone are the three most commonly known reproductive and sex hormones. (See Estrogens, Progesterone, and Testosterone for additional information.) These hormones work with other hormones in the endocrine system to regulate energy levels, metabolism, growth, stress responses, and reproductive health.
There are a number of ways to measure hormones (blood, urine, and saliva). It is very hard to get an accurate result from testing hormones. I had both saliva and blood tests, and they have both been completely different a number of times. Saliva testing is not very accurate, since very low levels of estrogen or progesterone are found in the saliva. Blood tests are more accurate, but the problem is that hormone levels can fluctuate from day to day and even from hour to hour, particularly in perimenopausal women. This makes the results hard to trust, so I have asked my primary care physician to run my hormones a few times within weeks of each other, and my results were the same each time. This gives me confidence that my levels are normal.
WARNING SIGNS OF HORMONAL IMBALANCE
Acne
Anxiety
Autoimmune diseases
Bloating
Body hair in excess
Bone loss (osteoporosis)
Breast cancer
Breast tenderness
Cancer
Candida overgrowth
Concentration difficulty
Depression
Diabetes
Eating disorders or extreme dieting
Endometriosis
Energy level low
Fatigue
Fibroids
Fibrocystic breasts
Hair is thinning
Headaches
Hot flashes
Infertility
Insomnia
Low libido
Menstrual irregularities
Mood swings
Night sweats
Obesity
Painful intercourse
PCOS (polycystic ovary syndrome)
PMS
Skin issues
Sleep issues
Thyroid disease
Uterine cancer
UTIs (Urinary Tract Infections)
Weight gain
KEY CONTRIBUTORS AND RISK FACTORS OF HORMONAL IMBALANCE
Dairy
Dairy increases estrogen levels.
Cow’s milk contains both estrogen and estrogen metabolites. Consuming cow’s milk products results in higher circulating estrogen levels. https://pubmed.ncbi.nlm.nih.gov/19496976/
Those who consume less dairy have a significantly lower risk of developing lung, breast, and ovarian cancer than those who consume more. https://pubmed.ncbi.nlm.nih.gov/25314053/
Dairy is a cancer-promoting food and it increases IGF-1 levels, which is a known cancer risk factor. https://pubmed.ncbi.nlm.nih.gov/31089868/
"Research on dairy confirms it causes disease and inflammation and it doesn't help to build strong bones." Fiber Fueled, Dr. Will Bulsiewicz
Choose plant milks over dairy when making smoothies, having cereal, making mashed potatoes, etc.
DIET
Women who have high estrogen levels due to their diet and lifestyle habits are at risk of developing cancer.
Eating a high-fat diet increases estrogen levels. https://pubmed.ncbi.nlm.nih.gov/8021957/ https://www.researchgate.net/publication/20382079_Nutritional_factors_associated_with_benign_breast_disease_etiology_A_case-control_study
Eating less fiber contributes to higher estrogen levels. https://pubmed.ncbi.nlm.nih.gov/8039147/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2744625/
Fibrocystic breasts
Many women have fibrocystic breasts and are not aware of it because they do not have symptoms. Other women experience swelling and generalized breast soreness, tenderness, or pain.
The condition often changes throughout the menstrual cycle, which means that abnormal hormone levels, particularly high estrogen, is a likely cause. Research supports this idea. In this study women reported breast pain after receiving estrogen or hormone replacement therapy. https://www.sciencedirect.com/science/article/abs/pii/S0002937899705600
Women who have fibrocystic breasts are at higher risk of developing breast cancer, especially if they have a family history of breast cancer. https://pubmed.ncbi.nlm.nih.gov/16034008/
HRT (hormone replacement therapy)
HRT drugs were developed by pharmaceutical companies to treat the unpleasant symptoms of diminished levels of estrogen, progesterone, and testosterone in women and men. Women in their 40s and 50s will generally have lower levels of estrogen and progesterone as they age and go into menopause, so many turn to HRT.
In the late 90s, HRT started becoming a concern, and by 2002 research showed that it caused more harm than benefit. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6780820/
Taking any type of HRT increases the risk of developing breast and ovarian cancers. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(19)31709-X/fulltext
Taking hormone replacement therapy after menopause can also suppress thyroid hormone levels and function. https://pubmed.ncbi.nlm.nih.gov/15142374/
Bioidentical hormones
Many women who are aware of the risk of HRT turn to bioidentical hormones, with the assumption that because they are natural, they must be safe.
Based on results of saliva or blood tests, a compounding pharmacy will use plant estrogens to create bioidentical hormones (chemically identical to what the human body produces) for an individual. There are two issues that can arise:
Compounding pharmacies are not always well-regulated.
Saliva and blood tests are not always accurate.
If you have warning signs that your hormones are out of balance, one of the best things to do is master your health routine (diet, hydration, exercise, de-stressing, and sleep). Visit the Thrive page to learn more.
Obesity
Excess fat in the body produces hormones. In essence, it is a poison carrier.
Fat cells are metabolically active and produce inflammatory cells and hormones that are converted to estrogen in the bloodstream.
This study shows that estrogen is synthesized in peripheral tissues such as adipose tissue (AT), which is body fat. https://pubmed.ncbi.nlm.nih.gov/33610799/
Obesity is the biggest driver of inflammation.
Oral contraceptives
Oral contraceptives have been available since the early 1960s, and are used by over 90 million women worldwide.
Oral contraceptives can increase breast cell proliferation. https://www.ncbi.nlm.nih.gov/books/NBK234347/
Younger users, ages 20-40, are at higher risk with long-term use. https://pubmed.ncbi.nlm.nih.gov/24633144/
Taking oral contraceptives can suppress thyroid hormone levels and function. Estrogen increases circulating levels of thyroxine-binding globulin, which decreases thyroid hormone levels and thyroid function. Thyroxine-binding globulin is the major transport protein for thyroid hormones around the body. https://pubmed.ncbi.nlm.nih.gov/4442279/
SMOKING
Chronic smoking can cause imbalance in endocrine homeostasis and impairment of fertility in both sexes. https://pubmed.ncbi.nlm.nih.gov/23173678/
This study of 684 healthy, fertile women showed considerable hormone interference due to smoking. https://pubmed.ncbi.nlm.nih.gov/1398476/
Toxins
Many chemicals, both natural and man-made, may mimic or interfere with the body’s hormones, known as the endocrine system. https://www.niehs.nih.gov/health/topics/agents/endocrine/index.cfm
These chemicals are called endocrine disruptors and include plastic bottles and containers, liners of metal food cans, detergents, flame retardants, food, toys, cosmetics, and pesticides.
Reduce your toxic load by eliminating toxins in your food, water, and air through the methods mentioned on this site. Visit the Detox page to learn more.
WHAT I’m DOING TO CREATE HORMONAL BALANCE
Besides irregular periods, I didn't have any other signs of hormonal imbalance when I was diagnosed with breast cancer, and perhaps that is because I was already living a healthy lifestyle. Yet, I decided to make more improvements to facilitate hormone regulation and ensure that excess estrogen was exiting my body. Before my diagnosis, I was diligent about diet and exercise, so I thought I was on the right track — but wow, I had so much more to learn! I have been extremely intentional in the areas below:
De-stress
Stress can lead to changes in the serum level of many hormones including glucocorticoids, catecholamines, growth hormone and prolactin. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3079864/
My Experience: Unfortunately, I was living in a perpetual state of stress leading up to the cancer diagnosis. One of the first things I began to practice in order to de-stress was to breathe deeply. Interestingly, right after my hysterectomy which forced me into menopause, I noticed that I could lessen the effect of a hot flash by deep breathing. When I learned the information about chronic stress and its impact, I think it confirmed for me that my healthy diet all of the years leading up to my cancer diagnosis may have actually saved my life. Visit the De-stress page to learn more.
DIET
Women who have high estrogen levels due to their diet and lifestyle habits are at risk of breast cancer. Research shows that the best approach for lowering estrogen levels is to adopt a low-fat, high-fiber, plant-based diet. https://pubmed.ncbi.nlm.nih.gov/2543203/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2223807/
Eat a low-fat diet.
A review of dietary intervention studies concluded that low-fat diets reduce plasma estradiol levels. https://pubmed.ncbi.nlm.nih.gov/10088623/
The lead author of this study concluded that maintaining less body fat, eating less fat, and eating more fiber resulted in lowering estrogen levels in post-menopausal women, which lowers their risk of breast cancer. https://pubmed.ncbi.nlm.nih.gov/21500098/
Eat a plant-based diet.
A case control study of women in Shanghai with fibrocystic breasts showed that a diet including more fruits and vegetables reduced the risk of proliferative and atypical lesions, which can reduce the risk of developing breast cancer. https://pubmed.ncbi.nlm.nih.gov/15522851/
In the study cited below, vegetarians had reduced levels of estrogen and increased levels of SHBG (sex hormone binding globulin), which helps to remove excess estrogen. The highest hormone levels were found in the meat eaters with breast cancer. Lower hormone levels reduce breast cancer risk. https://pubmed.ncbi.nlm.nih.gov/21500098/
Eat a high-fiber diet.
Women who eat a diet with inadequate fiber are at risk of having estrogen reabsorbed in the intestinal tract, rather than excreting the excess estrogen in their feces. Women are supposed to break down excess estrogen each day and excrete it in bowel movements. https://pubmed.ncbi.nlm.nih.gov/3628202/
Eating a low-fat, high-fiber, plant-based diet will help women eliminate excess estrogen on a daily basis. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3893100/ https://academic.oup.com/jnci/article/108/10/djw223/2412589
Eat soy.
This study shows that a diet including 1/2 cup of soy daily decreased hot flashes in women by 79%. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8462449/
Whole soy foods like soybeans and tofu protect against hormone-driven cancers by attaching these weak plant estrogens to receptor sites on cancer cells, effectively blocking the cells from being activated by strong estrogen. Soy phytoestrogens actually act as estrogen-blockers: “it appears that soy isoflavones do not function as an estrogen, but rather exhibit anti-estrogenic properties . . . soy isoflavones should be considered a potential anti-cancer therapeutic agent in hormone receptor positive breast cancer.” https://pubmed.ncbi.nlm.nih.gov/23919747/
Isoflavones have chemical structures that look a little like estrogen found in a woman’s body. However, phytoestrogens (isoflavones) are not the same as female estrogens. Soy foods don’t contain estrogen. https://www.oncologynutrition.org/erfc/healthy-nutrition-now/foods/soy-and-breast-cancer
Visit The Kitchen Treats member page to learn more about soy and how I consume soy each day.
Exercise
Exercise reduces body fat which produces estrogen-like hormone compounds. In his book Beating Cancer With Nutrition, Patrick Quillan says, “Hormones like testosterone or estrogen are not only produced by the gonads and ovaries, but are also produced by fat cells. So the more body fat a person has, the higher the likelihood of generating more tumor enhancing hormones.”
Exercise is an excellent form of detoxification, as toxins exit your body via sweat. Exercise also increases SHBG (sex hormone binding globulin), which binds to estrogens and deactivates them. Its function is to keep excessive free estrogen out of the bloodstream.
Exercise improves body composition. Lean muscle mass is the total weight of your body minus the fat. Do a combination of both aerobic (cardiovascular exercise) and strength training (push-ups, lifting weights, etc.) exercises to burn fat and build lean muscle mass, which increases metabolism and improves hormonal balance.
GUT HEALTH
The gut regulates hormones like estrogen. If the gut is unhealthy, it may flood the body with too much estrogen.
Women are supposed to break down excess estrogen each day and excrete it in bowel movements. If not, that estrogen can be reabsorbed and circulate back through the body. Estrogen is supposed to be carried to the liver and then excreted into bile, which then travels to the intestine, where it is excreted in feces. An unhealthy gut will not carry excess estrogen to the liver, but instead allow it to be reabsorbed into the bloodstream. https://pubmed.ncbi.nlm.nih.gov/3628202/
One study showed that women eating a vegetarian diet lower in fat and higher in fiber excreted three times more estrogen in their feces and had 15-20% lower plasma estrogen levels than women eating a westernized diet higher in fat and lower in fiber. https://pubmed.ncbi.nlm.nih.gov/7260944/
WEIGHT CONTROL
Lifestyle factors impact hormones, which regulate weight control. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3147122/
Hormones like testosterone or estrogen are not only produced by the gonads and ovaries, but are also produced by fat cells.
The more body fat a person has, the higher the likelihood of generating more estrogen-like hormone compounds and/or tumor enhancing hormones. https://pubmed.ncbi.nlm.nih.gov/34519778/